By addressing the genetic deficiency, allo-HSCT is a potentially curative option for patients with TDT1-3
By addressing the genetic deficiency, allo-HSCT is a potentially curative option for patients with TDT1-3
Many patients do not receive allo-HSCT due to the lack of suitable matched donor, presence of existing complications, or age1,3
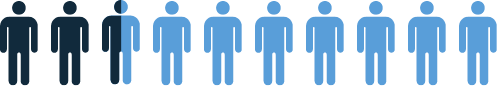
25% to 30%
patients have an MSD3
Optimal outcomes are achieved in pediatric patients who have an HLA MSD2,4
In recipients of matched sibling donor (MSD) transplants (n=1061), the results were markedly different than other donor groups, with OS and TFS 91 ± 1% and 83 ± 1%, respectively.4
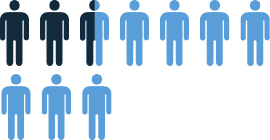
Survival for all
patients at 2 years4
Overall survival and thalassemia-free survival rates 2 years post-HSCT by donor type4
| Donor Type* | Overall Survival Rate† | Thalassemia-Free Survival Rate† |
|---|---|---|
| Matched Sibling Donor (n=1061) |
0.91 ± 0.01 | 0.83 ± 0.01 |
| Matched Related Donor (n=127) |
0.88 ± 0.04 | 0.78 ± 0.05 |
| Mismatched (n=57) |
0.68 ± 0.11 | 0.68 ± 0.11 |
| Unrelated Donor (n=210) |
0.77 ± 0.03 | 0.77 ± 0.03 |
†P<0.001
Survival outcomes in pediatric patients with an HLA MSD decreased with age4
| Age | |
|---|---|
| <2 years | |
| 2 to <5 years | |
| 5 to <10 years | |
| 10 to <14 years | |
| 14 to <18 years | |
| ≥18 years | |
| P-value (for trend) | P-value (for trend) |
| Overall Survival | Thalassemia-Free Survival | |||
|---|---|---|---|---|
| Number of Patients | Events | 2-year OS | Events | 2-year TFS |
| 66 | 3 | 0.95 ± 0.03 | 4 | 0.93 ± 0.03 |
| 266 | 13 | 0.94 ± 0.02 | 32 | 0.86 ± 0.03 |
| 352 | 33 | 0.90 ± 0.02 | 52 | 0.83 ± 0.02 |
| 197 | 8 | 0.96 ± 0.02 | 24 | 0.86 ± 0.03 |
| 97 | 14 | 0.82 ± 0.04 | 20 | 0.74 ± 0.05 |
| 82 | 16 | 0.80 ± 0.05 | 18 | 0.76 ± 0.05 |
| <0.001 | <0.001 | |||
HLA = human leukocyte antigen; MSD = matched sibling donor; OS = overall survival; TFS = thalassemia-free survival.
Adapted from Baronciani D, Angelucci E, Potschger U, et al. Hematopoietic stem cell transplantation in thalassemia: a report
from the European Society for Blood and Bone Marrow Transplantation Hemoglobinopathy Registry, 2000–2010.
Bone
Marrow Transplant. 2016;51(4):536-541.
HLA = human leukocyte antigen; MSD = matched sibling donor; OS = overall survival; TFS = thalassemia-free survival.
Adapted from Baronciani D, Angelucci E, Potschger U, et al. Hematopoietic stem cell transplantation in thalassemia: a report
from the European Society for Blood and Bone Marrow Transplantation Hemoglobinopathy Registry, 2000–2010.
Bone
Marrow Transplant. 2016;51(4):536-541.
A separate analysis demonstrated optimal outcomes of allo-HSCT in pediatric patients with an HLA MSD5
A separate retrospective analysis of 1100 patients (97% <16 years old) with beta-thalassemia major who underwent allo-HSCT between 2000 and 2016 in China, India, and the United States also demonstrated optimal outcomes are achieved within pediatric patients with an HLA matched sibling donor.
- For patients ≤6 years, patients aged 7 to 15 years, and patients aged 16 to 25 years, 5-year event-free survival was 86%, 80%, and 63%, respectively
- Compared with matched sibling transplants, there was higher risk of acute and chronic GvHD after mismatched related and unrelated donor transplants
There is limited experience of allo-HSCT in adult patients, as very few centers perform allo-HSCT in patients over the age of 18 years, and transplant-related mortality has persistently remained around 25%.3
Comprehensive, long-term follow-up after allo-HSCT is recommended to screen for complications6
Disease-related outcomes and late effects of allo-HSCT include6:
- Monitoring and management of mixed chimerism
- Iron overload
- Chronic GvHD
- Immune reconstitution and susceptibility to infections
- Screening for malignancies following exposure to transplant conditioning regimens and immunosuppression
The use of donor cells in allo-HSCT introduces the risk of potentially life-threatening and graft rejection.2,4,6
- Incidence of severe acute GvHD (Grade III–IV) can range from 9% to 17%, and approximately 5% to 9% of patients develop extensive chronic GvHD2,4
- TRM is an inherent risk for patients with TDT undergoing allo-HSCT, with a recent single-center study reporting an 11.6% rate of TRM7
- Graft failure occurs in about 20% of patients with TDT who undergo allo-HSCT6-8
| Severe Acute GvHD (grade III-IV)* |
9% (whole population) 7% (patients with HLA MSD)‡ |
| Limited Chronic GvHD† | 15% ± 1 |
| Extensive Chronic GvHD† | 6% ± 1 |
*Risk within first 100 days post-HSCT
†2-year risk post-HSCT
‡P=0.001
Chronic GvHD assessment was done in 1140 patients who survived with a functioning graft for >100 days.

Actor portrayal. Not a real patient.
Take the Beta-Thalassemia
Challenge